In the simplest sense of patient throughput, wireless technology can track the paths and wait times of patients through a care facility. However, to get the full value of patient throughput initiatives, wireless technology needs to be part of a holistic plan that addresses direct and indirect sources of delay.
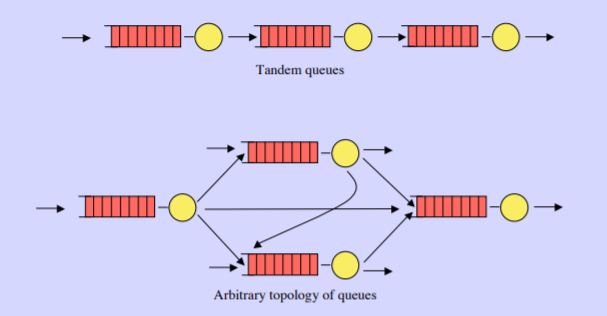
To borrow ideas from queuing theory, throughput is a function of arrival rate, service time and the resulting wait period. RTLS solutions provide real time insight to improve each of these steps, but there are other influences that are not technology related that should part of the larger strategy.
Arrival Rate’s Influence on Patient Throughput
Wireless wrist straps are provided to patients arriving at the healthcare facility providing a real time indication of changes in demand. But non-technology related techniques can be used to influence arrival rate.
- Coordinate with local communities, pharmacies, and secondary care facilities to address patient needs before they require hospitalization. This includes not only medical and trauma but mental health support as well.
- Proactively address hospital acquired conditions (HACs) like catheter-acquired infections and patient falls. RTLS solutions from AiRISTA provide hand hygiene solutions and patient wander management.
- Schedule elective surgery separately from emergency surgery to create a more predictable flow of patients downstream to ICUs and inpatient units.
Service Time’s Influence on Patient Throughput

Wireless asset tags are attached to equipment needed to treat patients. This ensures the right equipment and supplies are staged and ready when care providers arrive. Not only can you ensure availability of beds, pumps, etc., but RTLS solutions like those from AiRISTA can support workflows to ensure the equipment is sterilized and calibrated. Service time, as it relates to patient flow, can also be improved through redesign of processes and teamwork.
- Rather than treating triage as a location in the ED, streamline triage as part of thepatient intake process and convene physicians, PAs and nurse practitioners in the process for a single unified patient consensus.
- Create separate patient flows for emergent and nonemergent ED patients. Similarly, parallel OR suites for emergency surgical cases versus elective can streamline flow and maximize utilization.
Wait Period’s Influence on Patient Throughput
 Wireless wrist straps worn by patients track the location and time spent by each patient in the various stops through the hospital system. Real time alerts warn of excessive delays and long queues. Insights allow staff to dynamically shift resources to absorb surges and historical reports provide analysis for future improvements. But non-technology related techniques can be used to influence wait periods.
Wireless wrist straps worn by patients track the location and time spent by each patient in the various stops through the hospital system. Real time alerts warn of excessive delays and long queues. Insights allow staff to dynamically shift resources to absorb surges and historical reports provide analysis for future improvements. But non-technology related techniques can be used to influence wait periods.
- Change discharge procedures to reduce discharge delays by implementing medical readiness criteria in coordination with community services.
- A 2000-2003 study* of 120 ICUs in the US found that ED boarding for patients awaiting the ICU resulted in 10.7% ICU mortality for waits greater than 6 hours (vs. 8.4% for waits less than 6 hours). In-hospital mortality was 17.4% (vs. 12.9%).
To be most effective, patient throughput needs to be a sustained initiative that addresses bottlenecks to patient flow across the entire system. RTLS solutions like AiRISTA’s cloud RTLS platform is a technology component of a holistic approach. Cloud delivered RTLS addresses multiple use cases, with a simple interface, to coordinate cross functional teams and measure improvement.
* Chalfin D, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP; DELAY-ED study group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Critical Care Medicine. 2007





